Dr Bing Zhu
What is the difference between acute kidney injury and chronic kidney disease?
Within the names of the diseases, acute kidney injury implies a quick onset of disease, while chronic kidney disease suggests progression over a longer period of time. Acute kidney injury also has a high mortality of around 50%.
But beyond that, the more important distinction to make is that chronic kidney disease means the kidney dysfunction the patient has is permanent and irreversible. Whereas acute kidney injuries have a chance to recover – potentially back to normal kidney function. We have many cases of dogs and cats with creatinine levels over 800 that recover to non-azotaemic states, occasionally even with some decent concentrating ability.
However, to achieve this – the patient often requires a lot of veterinary support during the recovery phase and most importantly – initiation of these supportive measures must be done as soon as possible, before the damage caused by the acute kidney injury becomes permanent – meaning we are trying to prevent chronic kidney disease, or minimise the degree of chronic kidney disease a pet is left with.
Because of this chance for recovery – it is very important to distinguish between acute kidney injury and chronic kidney disease.
How can you tell the difference between acute kidney injury and chronic kidney disease?
An acute kidney injury means damage to the kidney occurring over a short period of time. There are various grades of acute kidney injury that one can look up on the IRIS website. Patients can have a significant acute kidney injury and not even be azotaemic (as we all know, we have to lose 75% of both kidneys before a patient’s creatinine will be outside the reference range). A good general rule of thumb is that a change in creatinine over about 30 points within a short period of time signifies some form of acute kidney injury.
Exactly period of time qualifies as a “short period of time” is a bit more complex. Certainly, if a patient sitting in hospital on IV fluids has a change in creatinine of about 30 points without a change in hydration status, then we can be confident there is an AKI occurring. This is even if the patient’s creatinine is within normal range (e.g. 50 to 80).
For outpatients, the suggestion is 3 months. This means that that providing hydration status and muscle mass remain the same – chronic kidney disease patients should not really have progression of their creatinine within 3 months. If they do have a jump up of 30 points within 3 months, then we need to be suspicious of an AKI.
The reason for suggesting “3 months” is that we often would recommend giving acute kidney injuries at least 3 months to see whether they will improve or not. If we give up (e.g. euthanise the patient, or condemn them to the diagnosis of “CKD”) before giving them 3 months of conditions supportive of renal recovery, then we really are not giving the kidneys a good enough chance to heal.
So any patient presenting with a new azotaemia that you do not have blood tests on in the past 3-6 months – you must consider that this patient could have an acute kidney injury. Assuming the patient has chronic kidney disease and treating as such may be robbing that patient of an opportunity to recover back to much better renal function.
However, even with lab-work documenting stable creatinines or SDMA over 3-6 months – unless a thorough work up is performed and appropriate treatment implemented, you can never be 100% sure that a patient truly has CKD or AKI.
As two examples, I have had a 12 year old labrador presenting with a creatinine of 180 who had had that level of azotaemia for over 1 year. This dog had an immune-mediated protein losing nephropathy that was diagnosed very late. We warned the owner that a lot of the kidney damage may be permanent already. However, when we treated the dog’s protein losing nephropathy, the dog’s creatinine retuned to below 140 and developed concentrating ability with specific gravities of 1.025.
Another example is a cat who had a creatinine of 200 for 6 months. Based on doing thorough investigations, it was found that this cat had significant intestinal disease that was causing it vomiting/diarrhoea, likely dehydration and secondary kidney issues. After treating the cat’s bowel disease, her creatinine returned to below 140.
These are 2 cases where even I myself would have suspected permanent damage, but yet again proves the remarkable recovery ability of the kidneys if given the chance. This means we must stop the rest of the body attacking the kidneys and give them time to recover.
Another general rule of thumb is that acute kidney injury patients tend to be sick (either from the acute kidney injury itself, OR from whatever disease is causing the acute kidney injury e.g. pancreatitis / bowel disease). Whereas chronic kidney disease patients tend to be very well in themselves and their disease is often discovered on routine general bloodwork (e.g. geriatric screening).
What are the first things that a primary care practitioner can do for a kidney disease case before referring it?
a) Full bloodwork – full blood cell count and full biochemistry (including cholesterol, bilirubin, CK, which are common missed on mini pre-GA panels).
b) Because of kidney disease patients’ predisposition to hypertension, an accurate blood pressure should be taken – ideally with owner present, with 8-10 readings while the patient is calm. Whether to trust the reading or treat borderline hypertension or not is a difficult to decide without knowing the patient and situation, but this information should ideally be provided in the referral history. Certainly if a calm patient is having a blood pressure over 170mmHg/180mmHg, treatment with amlodipine is often warranted.
c) Urine protein creatinine ratio to assess for proteinuria which has great prognostic and diagnostic/treatment implications. A cystocentesis urinalysis and culture should ideally be performed at an external lab to rule out pyelonephritis or interference of pyuria/bacteriuria on the UPCR.
d) It is not wrong to have a radiologist perform an abdominal ultrasound to assess the kidneys but primary care practitioners must keep in mind that these are expensive procedures and would likely need to be repeated after referral if there is suspicion of ureteral obstruction as we would need to assess the kidneys ourselves to evaluate whether surgery may be appropriate. Because these cases can be quite a financial burden on the owners, often it may be better for owners to have a discussion with a medicine specialist first before having the ultrasound performed and that the medicine specialist can be present for the ultrasound because our interpretation may be slightly different to the radiologist’s.
Are there any treatment strategies that should be implemented immediately?
Unfortunately, there is no easy answer to this question. Ultimately – treatment should be targeted at the cause of the AKI.
For example – if the AKI is caused by pancreatitis or bowel disease, putting the patient on a renal diet that is high in fat may be the worst thing possible and make the situation worse. If the patient is oliguric (which can be hard to tell initially), placing them on high rates of IV fluids may actually reduce GFR, cause interstitial oedema and delay renal recovery.
If a cat has an obstructed ureter – then surgery as soon as possible is recommended (delaying the procedure with days of IV fluids and blood draws usually makes them in a worse state for surgery so that decision/discussion needs to be made early on). The best treatment strategies are decisions made after a work up for what is the cause of the patient’s AKI.
The biggest piece of advice I can give is to discontinue any further damage to the kidneys, meaning: – discontinue kidney-toxic drugs such as NSAIDs, ACEI (unless treating proteinuria) – minimise heavy sedations unnecessarily – no elective anaesthetics such as dental procedures
What are the common errors made in acute kidney injury management or diagnosis?
The most common error made in cases that we see at SASH is owners being told their pet has “end stage kidney disease” or “chronic kidney disease” and started on a renal diet, when in fact the patient actually has an acute kidney injury. How severe the creatinine is on bloodwork does not necessarily predict whether a patient is likely to recover or not – that is more dependent on the cause of the acute kidney injury.
Another error commonly seen when vets are assessing patients with kidney disease would be whether or not the kidney failure is actually the cause of the patient’s unwellness. For example, we frequently see acute kidney injury secondary to pancreatitis or bowel disease. A pet may present for vomiting and poor appetite and on bloodwork have a creatinine of 180. It is very unlikely for mild azotaemia of that level to be the cause for severe vomiting and poor appetite, but some vets may think it is and prescribe a renal diet which is high in fat. The high fat diet may then make the pancreatitis or bowel disease worse and that in turn worsens the kidney disease.
The final common error frequently made in acute kidney injury is the volume of IV fluids. Without knowing exactly how dehydrated a patient is and what it’s ongoing losses and requirements are, it is impossible to tell exactly what rate of IV fluids a patient should be placed on. We can make a good “guestimate” using physical exam, tracking body weights and some bloodwork parameters – but ultimately it is a guess and we take a gamble and start them on a rate of fluids. However, for acute kidney injury patients, especially if polyuric or oliguric – the patient needs to be very closely monitored for overhydration or underhydration because any overhydration or underhydration can harm the kidneys and reduce changes of recovery.
This means monitoring their respiratory rate and effort every 2-4 hours and weighing them every 4-6 hours before and after urination and examining them multiple times a day to assess how their hydration is change with the initial “guestimate” rate of IV fluids administered. These are not patients where throwing them on IV fluids overnight without any monitoring would be appropriate if the owners are able to financially afford 24 hour care.
Often, we receive patients which are markedly overhydrated on IV fluids because they have been on “twice maintenance fluids” for a few days at their local vets. Overhydration actually causes interstitial oedema in the kidneys, reducing GFR and slows down renal recovery. Additionally if they have a condition they need surgery for (such as ureteral obstruction), the extra fluid in their lungs makes for an unstable anaesthetic.
What cases warrant referral? When should a case be referred?
For any case that is discovered to be newly azotaemic, the owners should be made aware that once bloodwork abnormalities are detected, the pet is only functioning on 25% of both their kidneys. They should also be made aware that this could either be an acute kidney injury or chronic kidney disease. Without a work up and following how the patient does over time, it is difficult to tell.
So for any newly azotaemic patients with dedicated owners who want to give their pet the best chance in case their pet does have an AKI, referral to an internal medicine specialist as soon as possible is appropriate. Of course, we also welcome CKD referrals, where we can meet the owners and set up a plan for management. As we discussed earlier, many cases can seem like CKD, but actually are patients undergoing constant AKIS – so any newly azotaemic patient being referred is never wrong!
What is “dialysis”? What cases warrant dialysis?
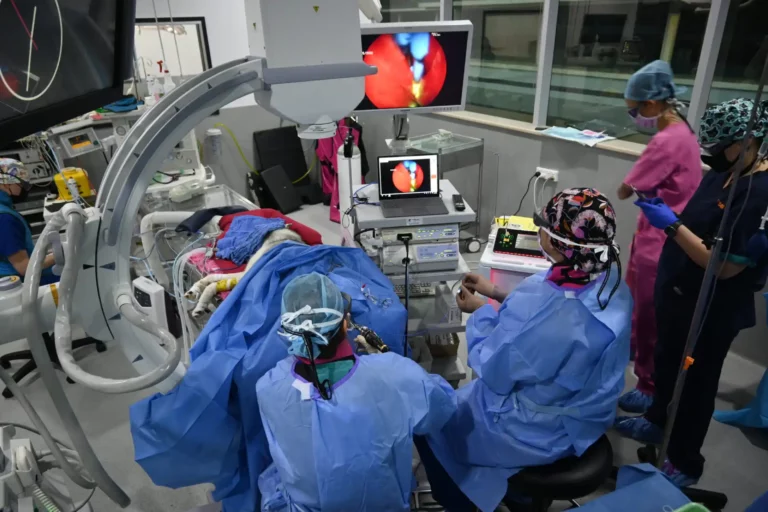
Dialysis is one of the many forms of extracorporeal renal replacement therapy where blood is taken out of a pet’s body, “cleansed” in a certain way, and returned to the pet’s body. There many different modalities of renal replacement therapy beyond dialysis and the purpose of these treatments is to act as a mechanical kidney for the dog or cat while its own kidneys are not working.
These treatments do not fix the kidney itself. It just buys time for the kidneys to heal. Acute kidney injuries can kill a patient within a few days to a few weeks. However, as we discussed earlier – we really need to give kidneys 3 months before we can say whether they will recover or not. Renal replacement therapies bridge that gap for us.
Generally, we recommend extracorporeal therapies if:
1) Patients are oliguric or anuric
2) The patient is fluid overloaded
3) The kidney disease is so severe that there are life threatening electrolyte abnormalities
4) The patient feels so unwell from its uraemia (constant vomiting, diarrhoea, bleeding, severe lethargy or neurological systems) that we would like to remove these toxins to make the patient feel better
5) There is a toxin we can remove (e.g. NSAIDs, ethylene glycol etc) – but these need to be performed as soon as possible after ingestion.
For ethical reasons, we generally do not perform “dialysis” for chronic kidney disease patients because our goal for all patients on extracorporeal therapies is to ultimately stop requiring these treatments, have their central lines removed, be eating and drinking and going back to normal quality of life. For chronic kidney disease patients, this is unlikely to occur and there are also ethical issues surrounding acquiring blood from donor pets for a terminal condition. In extremely rare cases, where a CKD dog’s quality of life is fantastic on dialysis and does not require frequent blood transfusions to have their dialysis treatments – chronic dialysis may be appropriate but we would need to assess these cases first.