Review by Dr Jana Leshinsky (Internal Medicine Specialist)
What is cat hyperthyroidism?
Cat hyperthyroidism occurs when the thyroid gland becomes “over active”. The thyroid glands are located in the neck and produce thyroid hormone. With hyperthyroidism, the thyroid gland becomes enlarged and produces excessive thyroid hormone. It is the most common hormonal disorder of cats and is a very common disease of older cats.
Cat hyperthyroidism symptoms
Cat hyperthyroidism results in a number of different symptoms and not all cats will have all of the following changes. In some cats, hyperthyroidism is diagnosed when the only clinical sign is weight loss. Other signs include:
- Increased vocalisation
- Fast heart and breathing rates
- Increased appetite and weight loss
- Increased vomiting and diarrhoea
- Increases in thirst.
Hyperthyroidism can be effectively treated, but left untreated it becomes life threatening. Untreated cats can develop heart disease, and problems with blood pressure, the kidneys and the heart.
Cat hyperthyroidism treatments
There are different approaches to treating hyperthyroidism:
1. Daily control of thyroid hormone production
Although effective in alleviating the symptoms associated with hyperthyroidism in cats, these options do not cure the underlying condition, so treatment is life long. These treatments can be expensive over time and are mainly recommended for cats with substantial, concurrent disease that may prohibit more curative treatments.
There are 2 ways of controlling daily thyroid hormone production:
a) Daily medical management
There are anti-thyroid prescription drugs available that block the production of thyroid hormone. It is quite common to need increased doses overtime, and depending on the specific drug, efficacy can be variable.
Anti-thyroid medications can have side effects. The most common are mild and resolve without needing to stop treatment (such as vomiting, diarrhoea, loss of appetite). However they can sometimes cause more serious side effects such as liver toxicity, skin conditions and low white blood cell counts, which would require discontinuation of use. Cats on daily medication require check ups and blood tests to ensure the dose is adequate and there are no adverse effects of the medication.
b) Dietary therapy
There are also specific commercial prescription diets available that that reduced thyroid hormone production by restricting iodine (a nutrient needed for the production of thyroid hormone) in the diet. Studies suggest > 82% of cats will respond to the diet. However, the diet must be strictly adhered to (with no other foods given), and its long term safety is unknown.
2. Treatments that cure cat hyperthyroidism
a) Surgery
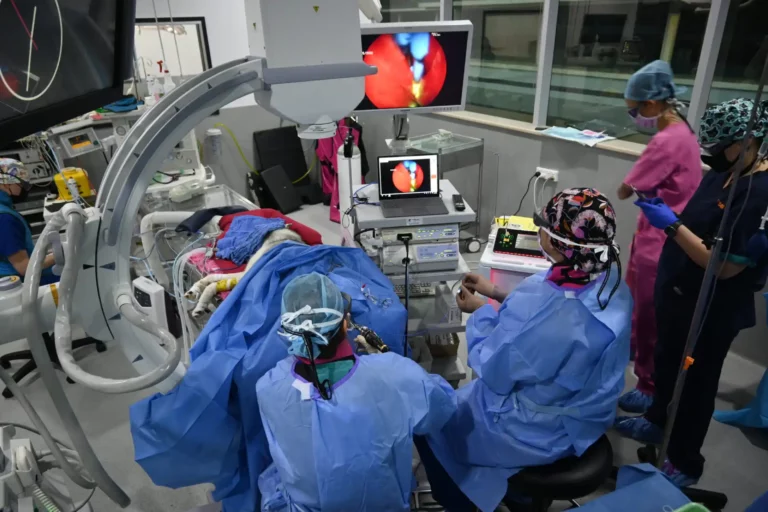
Surgical removal of the thyroid gland can be performed and can be an effective treatment. However, there are risks and complications involved with anaesthesia in older cats and there are risks of damaging the parathyroid gland which sits near the thyroid gland and controls blood calcium levels. For this reason, if this option is to be explored, it should be performed by a Specialist Surgeon working with a Specialist Anaesthetist.
b) Radioactive iodine treatment
Radioactive iodine (or radioiodine) treatment is recognised worldwide as being the gold standard treatment for hyperthyroid cats. Studies show that cats treated with radioactive iodine live longer than those treated with daily medical management. The radiation is concentrated in the thyroid gland, destroying the overactive tissue whilst having no adverse effects on the rest of the body. In ~ 95% of cats, a single treatment, administered by a single oral capsule, can cure hyperthyroidism. It is also a very safe treatment with minimal side effects.
Due to radiation safety regulations, cats undergoing this treatment needs to be hospitalised for a week following treatment. Only a small number of facilities offer radioactive iodine treatment and SASH is one of these facilities.
Benefits of radioactive iodine for cat hyperthyroidism
Benefits of radioactive iodine treatment for cats include:
- No daily medication/special diets and their associated side effects
- No close monitoring and regular blood tests
- Less likelihood of increasing difficulties in management, possible with daily medical management
- Safe way to cure the condition without general anaesthesia
Cat hyperthyroidism treatment costs
At first glance, daily medical management of cat hyperthyroidism appears attractive as it seems to be a much cheaper option. However, because the treatment is lifelong, costs quickly add up associated with on-going:
- Monitoring/testing
- Prescription drugs/food
- Potential complications & additional associated costs
Typically, the cost for treating a cat over a one-year period is similar to the cost of radioactive iodine. Therefore, radioiodine is an extremely cost effective treatment except in situations where the cat has concurrent diseases making it unlikely to survive beyond the next year. Most cats with uncomplicated hyperthyroidism will live several years following radioiodine treatment, unless they develop another disease.
Why choose SASH for your cat’s radioiodine treatment?
The assessment and treatment of your cat will be overseen by one of SASH’s world-class Internal Medicine Specialists, in a state-of-the-art radioiodine treatment and after facility. SASH also has a team of specially trained Feline Nurse who are available for cat patients. When necessary, the Internal Medicine team will also work closely with other in-house specialists in departments such as Opthalmology, Surgery, Anaesthesia, and Critical Care. This cross functional collaboration is essential for patients with complicated or multiple medical requirements that would benefit from not one, but a whole team of experts.
To decrease the stress of hospitalisation, the comfort of your cat is of the highest importance. SASH was the first hospital in Australia to be awarded a gold level “Cat Friendly Clinic” accreditation with the International Society of Feline Medicine. As part of this accreditation, SASH has a quiet and welcoming Feline Ward, reserved only for feline patients. Great pride is taken to ensure care and treatment is personalised for each individual cat, especially senior patients and those with special needs, and we encourage you to bring their favourite foods.
SASH works very closely with your local vets to keep them updated on your cat’s condition, and collaborate with follow up treatment. The SASH specialists are also available to provide on-going support for your local vet if they have questions about the long term care of your cat after treatment.
If your cat has been diagnosed with hyperthyroidism or you suspect it may have hyperthyroidism, click the contact link below to book an appointment with the SASH Internal Medicine team.